Don’t Ignore ACA Compliance Requirements
Following the Supreme Court’s June 2021 decision in California v. Texas, which rejected a challenge to the constitutionality of the Affordable Care Act (“ACA”), the often-debated statute has largely remained out of the news.
Following the Supreme Court’s June 2021 decision in California v. Texas, which rejected a challenge to the constitutionality of the Affordable Care Act (“ACA”), the often-debated statute has largely remained out of the news. Contractors should not ignore the ACA requirements simply because the ACA has been out of the news.
With the statute intact, covered employers throughout the U.S. remain subject to the ACA’s employer shared responsibility provisions, which include the employer mandate and information reporting requirements. While these requirements have been in effect since 2015, ensuring compliance is more important now because the IRS is increasing enforcement activities and no longer offering good-faith relief from penalties under IRC Sections 6721 and 6722 associated with furnishing or filing an incomplete or inaccurate information on Forms 1094 and/or 1095.
Considering these developments, it is critical that all employers with 50 or more employees place a renewed emphasis on ACA compliance, particularly with respect to the accuracy and completeness of the information contained on 1094-C and 1095-C forms submitted to the IRS and employees.
Background on the ACA Employer Mandates:
Which Employers Are Covered By the ACA? Under the ACA’s shared responsibility provisions, all applicable large employers (“ALEs”) must offer their full-time employees affordable health insurance coverage that constitutes minimum essential coverage and provides minimum value, or risk being subject to penalty. For purposes of the ACA, ALEs are employers who had an average of 50 or more full-time or full-time equivalent employees during the prior calendar year. To be considered a full-time employee under the ACA, an individual must generally average at least 30 hours of service per week or 130 hours of service in a given month.
Penalties are Potentially Significant. ALEs may be subject to significant penalties under the shared responsibility provisions for either: (a) failing to offer qualified coverage to 95% of full-time employees in any month (the “A” penalty); or (b) by offering otherwise qualifying coverage that is not affordable or does not meet certain minimum value thresholds (the “B” penalty). If incurred, the “A” penalty is levied against the ALE’s entire employee base, and for 2022 is calculated as follows: (Total # of ACA FT employees – 30) x $229.17 per month or $2,750 per year. As for the “B” penalty, this is assessed on a per employee, per month basis for all months that an employee declines coverage and obtains subsidized coverage elsewhere. For 2022, the “B” penalty is calculated on a per employee basis at a rate of either $343.33 per employee, per month or $4,060 per employee, per year. Where an employer is assessed a penalty under the shared responsibility provisions, the IRS will issue a Letter 226-J, providing notice of potential liability based on the IRS’s analysis of, among other things, information contained on Forms 1094-C and 1095-C filed by the employer. Employers are permitted 30 days to respond, and if contesting the proposed penalty, must provide supporting information.
Separately, ALEs may also become subject to penalty for failing to comply with the ACA’s information reporting requirements under Sections 6721 and 7622. Under these provisions, an employer may be subject to penalty for furnishing or filing a Form 1094-C or 1095-C that was untimely, incorrect, or incomplete. The penalties associated with an untimely, incorrect, or incomplete form are $280 per form furnished to an employee and $280 per form filed with the IRS, resulting in a potential combined penalty of $560 per employee. ALEs that fail to comply with the information reporting requirements will receive either a Letter 5005-A or Letter 927-CG depending on whether the employer’s filing was late, incorrect, incomplete, or not submitted at all.
Recent Increased Risk of Penalty:
IRS Enforcement Activity. Since the relevant provisions of the ACA became effective in 2015, the IRS’s enforcement efforts have often been delayed by a matter of years; however, with a no limitations period associated with most penalties under the ACA, this delay has not insulated ALEs from liability. Moreover, the recent uptick in penalty notices suggests that the IRS’s ability to analyze covered employer’s compliance with the information reporting requirements has improved.
Elimination of Transitional Good-Faith Relief. Under the regulations applicable to the ACA’s shared responsibility provisions, transitional good faith-relief was made available to the penalties under Sections 6721 and 6722 for furnishing/filing incorrect or incomplete information where an ALE could demonstrate that it made a good-faith effort to comply with the information reporting requirements. With the protection of this transitional relief, many entities focused predominantly on simply furnishing and filing all forms before the applicable deadlines, placing significantly less emphasis on the accuracy or completeness of tine information being provided. Going forward, it is critical that employers place an enhanced emphasis on ensuring that all forms are not only furnished and filed in a timely manner, but that the information is both correct and complete. Failure to do so will open many covered employers to significant new liability.
Best Practices for Avoiding Penalties:
Ensure timely, complete, and accurate reporting. While many employers have developed a certain level of familiarity and comfort with the employer shared responsibility provisions, and what actions must be taken to avoid liability under the “A” and “B” penalties, the information reporting requirements remain a source of confusion to many. Without the protection of the transitional good-faith relief, it is advisable for all covered employers to carefully assess the adequacy of their current ACA reporting process. This should include a comprehensive review of the validity of data being utilized and the accuracy of the code determinations.
Audit all prior ACA filings. Employers may correct prior submissions at any time before a penalty notice is issued by the IRS. Conducting a review of prior filings may uncover incorrect or incomplete returns that can be addressed before such issues potentially result in the issuance of a Letter 226-J.
Establish a comprehensive, monthly process for ACA compliance. Penalties under the ACA may accrue on a monthly basis, but many employers view ACA compliance as an annual activity. To ensure compliance with both the employer shared responsibility provisions and the information reporting requirements, it is critical to approach ACA compliance from a monthly perspective, as doing so provides the opportunity to identify and remediate issues in real time, when steps can be taken to minimize or eliminate any potential liability.
Bill Lowe is an attorney with Bolanos Low in Pittsford, N.Y., specializing in labor and employment law. Reach him at 585-643-8440 or through www.bolanoslowe.com.
Published: May 9, 2022
IN THIS ISSUE
2022 Brings New Compliance Challenges and Financial Strategies
As the construction industry focused heavily on pandemic-related changes over the past two years, other necessary changes were created or delayed.
Capitol Hill Update: SMACNA's Take on 2022 Funding Bill, Davis-Bacon Regulations, PLAs
As Congress has been working through its priorities and dealing with the ramifications of the Russian invasion of Ukraine, SMACNA has been active on the issues important to SMACNA contractors.
CEO Update: Building on SMACNA’s Strengths
It has been a very productive four months since I started in January as SMACNA’s CEO.
Copper Soldering Strike Force Team Prepares Michigan SMACNA for Success
ITI strengthens copper training to help prep Custom Architectural Sheet Specialists for historical restorations.
Don’t Ignore ACA Compliance Requirements
Following the Supreme Court’s June 2021 decision in California v. Texas, which rejected a challenge to the constitutionality of the Affordable Care Act (“ACA”), the often-debated statute has largely remained out of the news.
Guarding Against Risk Through a Structured Client Selection Process
It has long been an axiom that more industry firms go bankrupt during expansionary periods than during recessionary ones and that firms are more likely to fail due to cash crises than profitability problems.
High Quality Performance Leads to Years of Work
Quality work builds long-term, repeat business for Artlip & Sons in Chicago.
How to Get Your Business Seen First in Google Searches
How Search Engine Optimization helps local consumers find your HVAC business.
President's Column: A Workforce Shortage Solution
Our trade has a certain rhythm to it. From proposals to pipelines to projects, there is a routine that keeps our businesses humming.
Running on Fumes Management
Fabricating ductwork for industrial fume management requires special knowledge. Indiana SMACNA member Vidimos Inc. talks about the challenges and opportunities these types of projects bring.
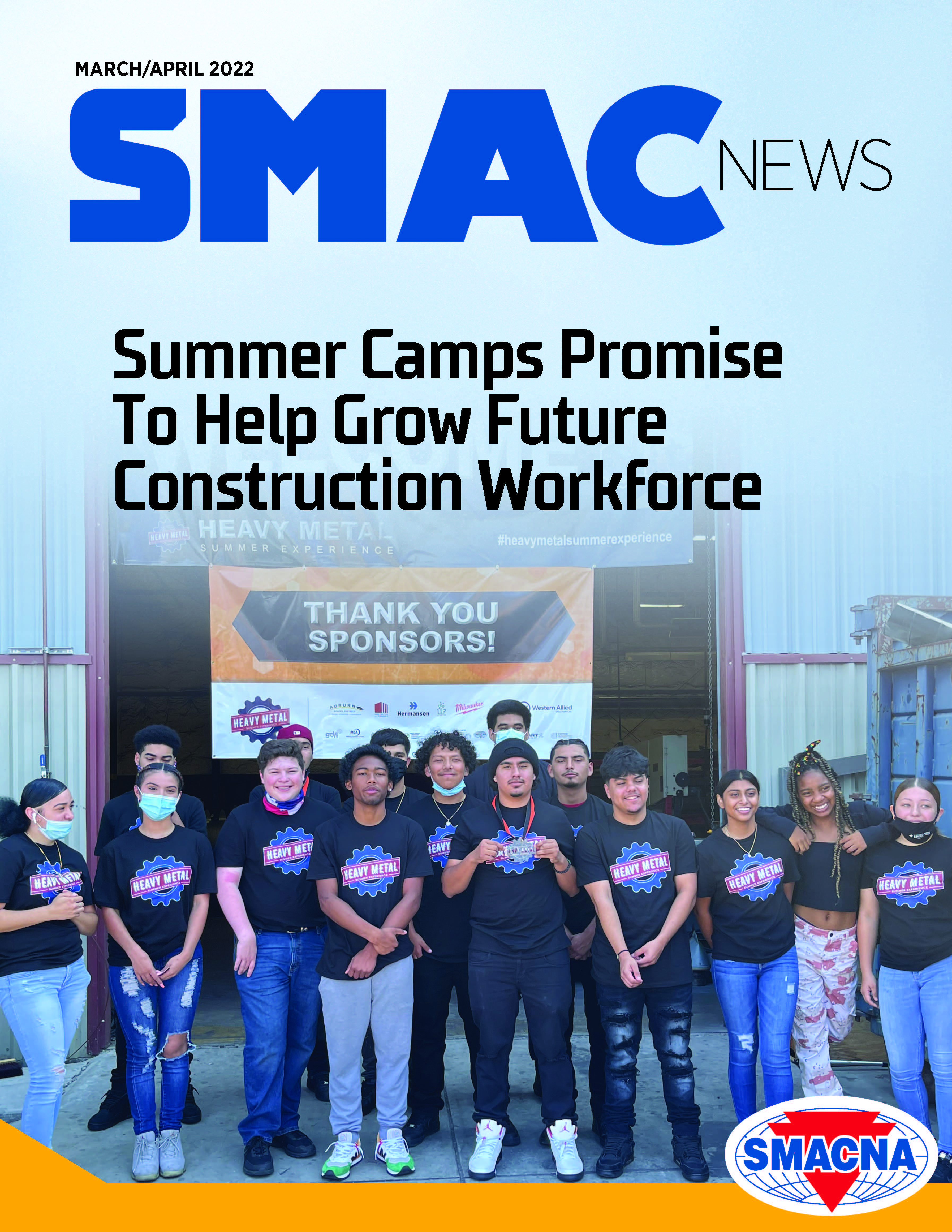
Summer Camps Create Opportunities to Grow Construction Workforce
As the labor crisis looms, companies focus on building a new generation of industry leaders.
Welcome New SMACNA Members
Welcome New SMACNA Members
Wisconsin Junior Hockey Team Honors Union Trades
Players learn important skills on and off the ice.